By IMAGE
15th Feb 2022
15th Feb 2022
Sponsored By

Not sure what a follicle stimulating hormone is? What's the difference between certain fertility tests and treatments? We explain common fertility terms in this helpful reference guide.
When starting your fertility journey, it can sometimes feel like a game of catch up. There’s a whole world of information out there, and an entire community discussing health issues and treatment options in scientific terms, acronyms, and unfamiliar words. It can even feel like a whole new language.
That’s why we’ve worked with Ireland’s leading fertility clinic, Waterstone Clinic, to create a beginner’s guide to fertility terms, so you can have a helpful head start with real definitions while you find your way and make decisions.
“Whatever stage you are at on your fertility journey, being equipped with knowledge and understanding will help make the process less mysterious,” explains Mary McAuliffe, Head of Clinical Services at Waterstone Clinic.
Below, we break down common fertility terms you’ll most likely hear from medical professionals and find on internet searches, and explain what tests and treatments are. Starting this journey, you’ll be TTC (“trying to conceive”) — a term often used in fertility forums to describe a stage of the fertility journey, letting others know that you are currently preparing to become pregnant.
Fertility testing
Starting out, whether you’re on a journey to parenthood or just interested in having your fertility checked, you’ll hear about these tests:
Anti-Müllerian Hormone (AMH): The AMH test is a reliable test of your ovarian reserve and can give an indication of the number of eggs are in your ovaries and whether it is average for your age. Your result will tell you if your fertility can be classed as good or poor for your age range. An AMH blood test should be read alongside an antral follicle count during a fertility focused ultrasound scan, so that the result is in context. Your AMH level will help you make decisions about your fertility journey and what treatment (if any) might be recommended to you.
Transvaginal Ultrasound (TVUS): During your assessments, you will have a transvaginal ultrasound. The ultrasound is fertility focused and is an internal scan using a probe. This ultrasound will help identify any cysts on your ovaries, and the health of your uterus and pelvis.
Antral Follicle Count (AFC): During your fertility-focused ultrasound scan, the fertility specialist will examine your ovaries and uterus and will be able to count the number of tiny follicles within each ovary (a follicle is a tiny bubble of fluid that contains an egg). This count is an antral follicle count and, together with your AMH result, gives the specialist an insight into how your fertility is for your age. If you need to proceed with treatment, these tests (AMH and antral follicle count) can help target the amount of medication you need.
Hormone Profile: A hormone profile is a collection of blood tests (generally taken at the beginning of your cycle) that test a range of hormones that are important for fertility. Usually, this would include FSH (follicle stimulating hormone), LH (luteinising hormone), E2 (oestradiol) and thyroid hormones. Occasionally, when you’re having these blood tests taken, your team might take the opportunity to take tests like rubella immunity as well.
Semen Analysis (SA): A semen analysis is a male fertility test. A sample of semen is tested for the number of sperm that are present per millilitre of the sample. The sperm are observed under the microscope to examine what percentage of them are moving as they should, and what percentage of them have a normal shape. Most semen analysis result sheets will also detail what the normal range for each of these measures are, and what the specialist’s recommendations are.
Terms from treatment
If you need some assistance to build your family, there is a range of options available, depending on your needs. Throughout treatment, you’ll hear a lot of biological and scientific terms. Here are some common ones:
Follicle: These are very important in fertility treatment! Follicles are tiny bubbles of fluid in the ovary that each contain a developing egg. There are a number of follicles available during each cycle that may be selected (under the control of follicle stimulating hormone) to develop and mature. One will ovulate and release the egg from your ovary and into your fallopian tube during ovulation. In treatment cycles, depending on the treatment type, medication will encourage a number of follicles to grow, and you will have scans to track these developing follicles until they reach maturity and are ready for either ovulation or egg collection.
Follicle Stimulating Hormone: This hormone, which is produced by the pituitary gland in the brain, encourages and selects one follicle to grow in a natural cycle. In fertility treatment, a synthetic version of this hormone is used in a higher dose than the body would produce in order to get a number of follicles growing simultaneously. This will increase the chance of pregnancy in ovulation induction or IUI cycles, or increase the number of eggs available for an IVF cycle. This medication is given in injection form, taken just under your skin. It’s usually taken for eight to 12 days, depending on how the follicles grow.
Embryo: Once an egg is fertilised by sperm and begins the process of cells dividing and multiplying, it becomes an embryo. After five to six days of growth, the embryo development has reached hundreds of cells and is called a blastocyst.
Embryo Transfer: An embryo transfer routinely takes place in an IVF cycle on Day 3, 5 or 6. The embryo is loaded into a fine plastic tube and is passed inside the uterus. The procedure feels a bit like a smear test.
Cryopreservation: This is the general term for freezing. Sperm, eggs and embryos can all be cryopreserved for later use.
Vitrification: This is a specialised, ultra-fast technique for freezing embryos and eggs. It is so fast that it allows no time for ice crystals to form, so it is more safe for the eggs and embryos.
Treatment
Fertility treatments are usually referred to by their acronyms (like “IVF”). The team will make recommendations on which they feel is the most appropriate for your situation based on your test results.
Ovulation Induction (OII): OII is a treatment to help you ovulate. The medications help to stimulate the release of the follicle stimulating hormone (FSH) needed to develop a follicle in the ovary. When the follicle is the right size, ovulation is induced by an injection under your skin, and the couple are advised to have intercourse around the time of ovulation. This treatment is often suggested to couples where the female partner doesn’t ovulate regularly and it increases their chances of pregnancy.
Intrauterine Insemination (IUI): IUI is a simple fertility treatment where the ovaries are mildly stimulated with medication to encourage the growth of a small number of follicles. Ovulation is triggered, and a sample of sperm (from a partner or donor) is loaded into a plastic tube in the laboratory and is passed into your womb on your most fertile day. Similar to an embryo transfer, the procedure feels much like a smear test.
In-Vitro Fertilisation (IVF): Probably the most well known fertility treatment, IVF is a high-tech process. A patient will take medication to stimulate the ovaries and when the follicles reach the right size, the eggs are collected from the ovaries. In the laboratory, the eggs and sperm (from a partner or donor) are placed together to achieve fertilisation. The fertilised eggs develop into embryos and are then transferred back into the uterus in an embryo transfer procedure. IVF is suitable for a wide range of fertility issues and is one of the most successful treatments available.
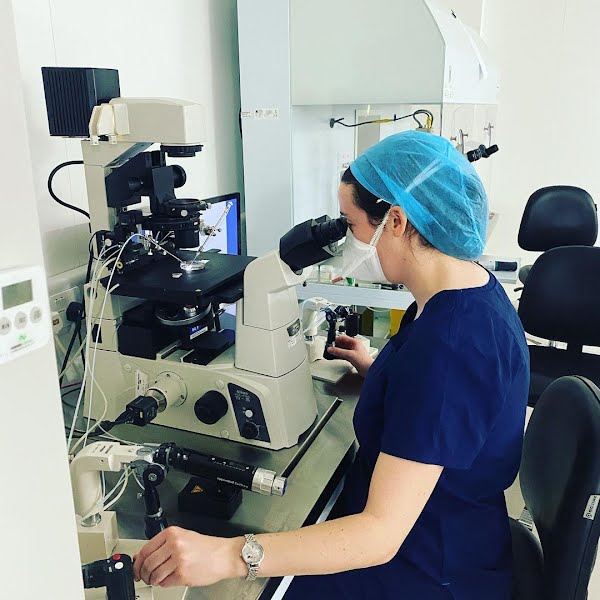
Intracytoplasmic Sperm Injection (ICSI): ICSI treatment is a form of IVF treatment with a specialised fertilisation procedure. It is used when there is a low number of sperm in the sample and when there is a concern that the sample may not fertilise the eggs available. Once the eggs are collected, instead of placing the sperm with the eggs as in traditional IVF, an embryologist injects each mature egg with a single sperm under a high powered microscope.
Frozen Embryo Transfer (FET): When patients have an IVF or ICSI cycle, they may have additional embryos remaining after an embryo was selected and used in an embryo transfer. The additional embryos can be frozen for future use. Many patients can then build their family from one cycle of IVF. In a frozen embryo transfer cycle, the patient will take medication to thicken the lining of the womb, and once the lining is ready, the medication is changed to plan for embryo transfer. On the day of the transfer, the embryos are thawed and then transferred to the uterus in an embryo transfer procedure.
This glossary can be a helpful guide when navigating your fertility journey, and as Mary McAuliffe of Waterstone Clinic advises, “If there is ever any term or anything you’re unsure of, just ask your team. We are here to guide you.”
Continue to follow us here to hear from Ireland’s leading experts in our IMAGE talks Fertility series in partnership with Waterstone Clinic.