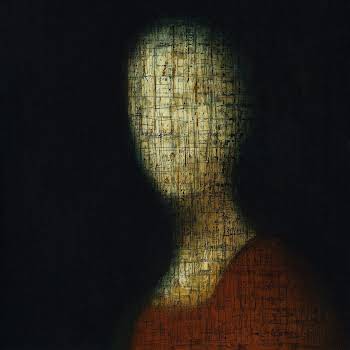
Working in palliative care: ‘The majority of people are peaceful as death approaches’
By Lia Hynes
20th Sep 2018
20th Sep 2018
In advance of this Thursday’s Ireland’s Biggest Coffee Morning for Hospice Together with Bewley’s, a member of the palliative care team from Our Lady’s Hospice in Harold’s Cross describes the work involved in guiding someone on their final journey.
Noreen Holland is Assistant Director of Nursing for Palliative Care at Our Lady’s Hospice Harold Cross. She has worked in all areas of palliative care and has been in her current role, managing and leading the nursing team, looking after the in-patient unit, the day hospice facility, and two Community Palliative Care (mobile) teams working out of Harold’s Cross, for eight years.
“I love my job,” she reflects. “I knew very early on in my nursing career that I was a medical rather than a surgical nurse. As a medical nurse, you are looking after patients that are sick and in need of conversation, engagement, more than a surgical nurse, who is involved with the patients who have their surgery and then go home.”
Related: Sentenced to death by cancer
Originally, she worked in children’s nursing, where communicating with the family, rather than just the patient, is a feature of the job.
“When I moved to do my general nursing I found it very strange that I was only dealing with the patient; the family were largely excluded. More senior colleagues said to me ‘you’re very good with dealing with someone who is dying, and you’re not afraid of talking to the family’. And I wasn’t. So I wrote to the hospice and asked if I could come to work there. ”
Naturally, the work is challenging, but never overwhelmingly so. “Because it was what I wanted to do I was never afraid, I never found it daunting.”
“People would often say that’s very hard work, but actually the feedback you get from patients and families is energising. I would go home from my shift physically very tired, but not depressed or down. Because I felt I was helping people to be in a better place.”
Truthful, open and honest
“We would have patients who would be very fearful of the suffering that might be ahead of them. As a team, we make every effort to make them as comfortable as we can”
Fear is something that Noreen and her colleagues commonly assist new arrivals in managing. “We would have patients who would be very fearful of the suffering that might be ahead of them. As a team, we make every effort to make them as comfortable as we can, to answer their questions, and to help them reframe their thinking so they gradually become less frightened. People do settle in their life journey, they settle in their minds.” Knowing they will not be left in pain helps hugely, she explains.
Patients are typically admitted for one of three common reasons. Symptom management- pain, anxiety- which will require a stay of a few weeks until these issues have been brought under control, before returning home. Respite care, and end of life care.
Related: ‘If love could keep Rachael alive, she would have lived forever’
“Most people do know when they reach us that they’re terminally ill. There was a time when people would arrive and they wouldn’t have been told that they were coming to the hospice. It was meant well in that families were protecting the individual from the fear of the hospice, but actually, we find that collusion doesn’t help. We would always encourage families to be truthful and open and honest. No matter how bad the truth is, it’s never as bad as what people imagine might be happening. And patients have told us that; I’m glad now I know the truth, because now I know where I stand, that kind of thing.”
Honesty and information are key to helping families cope and preparing them for the change.
Peaceful as death approaches
“Some would feel the presence of other family members who had died. Occasionally we have people who would have great difficulty accepting what is happening, and up until the end they are restless and uneasy.”
“Nurses and doctors who are experienced in working with people whose life is ebbing away will notice changes happening, and will advise a family so that they can be prepared. That preparedness gives them the strength and the confidence to keep going.”
“It’s not that we can predict everything, but we notice the subtle changes. It might be just that there is less energy, or that the person is taking less food. That their pallor is changing or they’re a little bit more short of breath. Sometimes the person will notice it themselves, and they’ll begin to distance themselves a little bit from those around them. Particularly I’ve noticed that mothers do that; they’re preparing the children- and sometimes these are adult children- for the break. They’ll say things like ‘you don’t need to come in now every day’, or ‘you don’t need to come in until six o clock’. Some people can plan and organise how they want everything to be managed, it’s amazing. That’s why the work is so special. You can see people determining their own journey.”
Related: ‘I’ve less than a year to make memories with my son’
The majority of people are peaceful as death approaches, Noreen reflects. “Some would feel the presence of other family members who had died. Occasionally we have people who would have great difficulty accepting what is happening, and up until the end they are restless and uneasy. We find that difficult, because we perceive that as someone not having had a good death. If we are dissatisfied with how someone dies – will have a case review to see if we can learn and put things right for the next time. But sometimes there are elements that we can’t control.”

The not knowing can be very scary
There are several important characteristics of a palliative carer. “You need somebody who’s well able to care for themselves, who is resilient, strong, compassionate, caring and confident. It’s important that staff have their breaks, and their holidays, and get away from this. People who are well able to plan their weekends and their holidays are more resilient when they’re back on duty. There is a professional boundary that shouldn’t be crossed. Where a member of staff gets too involved they can become quite stressed – when personal feelings become confused with professional challenges.”
On occasion, people will express regrets towards the end, but the team works to manage these thoughts. “You hear things like ‘I wish I’d retired younger; I only got to enjoy a few years of my retirement’. Or ‘I wish I’d changed my job’. Work, lifestyle, and relationship stuff. While we can’t change the past, we try to help people look at what is good, even small things, when they’re feeling down. They might be talking about having worked hard and you might remind them that they have a lovely family coming into them. Research about quality of life at end of life suggests that those who focus on the here and now and don’t look too far ahead report a better quality of life. Therefore, we encourage people to focus on achievable goals.”
Related: How to grieve in a society disconnected from death
On helping children to cope with death, the hospice encourages families to bring them in to visit their loved one, to “let them see for themselves the changes that are happening. Our social worker would work with children, give them time to express their feelings verbally or though art sometimes. I think bringing children to a funeral is the right thing to do, so that they are able to be part of the ritual, and say their goodbyes. I think it’s the collusion and the hiding that causes more anxiety for people. They may think ‘well it must be really bad if they’re hiding this from me, what was it that I couldn’t see?’ Whereas if they see it for themselves they know the reality of the situation then, and sad as it might be, it’s probably less worrying than not knowing. The not knowing can be very scary.”
Ireland’s Biggest Coffee Morning Together With Bewley’s
Thursday 20th September is the 26th year of this nationwide campaign to help raise vital funds for local hospice and home-care services. Over €35 million has been raised by people around Ireland so far. The money raised is crucial to ensuring that we continue to meet patients’ needs and support families.
How to take part
People can help to make a difference in someone’s life by hosting a coffee morning to help raise funds for their local hospice and home-care service. You can register at www.olh.ie/coffee or by calling 1850 660 606. Alternatively, text COFFEE to 50300 to donate €4*
When you register, you will receive a pack from Our Lady’s Hospice & Care Services containing Bewley’s coffee, posters, collection boxes, tent cards and invitations free of charge. You have the choice of ground coffee (suitable for cafetieres), instant coffee, or if you prefer – some of each.
You can invite friends, family, co-workers or club-mates to join you for a cup of coffee on Thursday the 20th of September (or any date that suits you). Some people add a bit of excitement to the day with cakes and bake-offs, competitions or raffles. Finally, we ask that you donate the proceeds to Our Lady’s Hospice & Care Services, where your funds will make a huge difference.
*Text costs €4. Ireland’s Biggest Coffee Morning for Hospice Together with Bewley’s will receive a minimum of €3.60. Service Provider: LIKECHARITY. Helpline: 076 6805278.