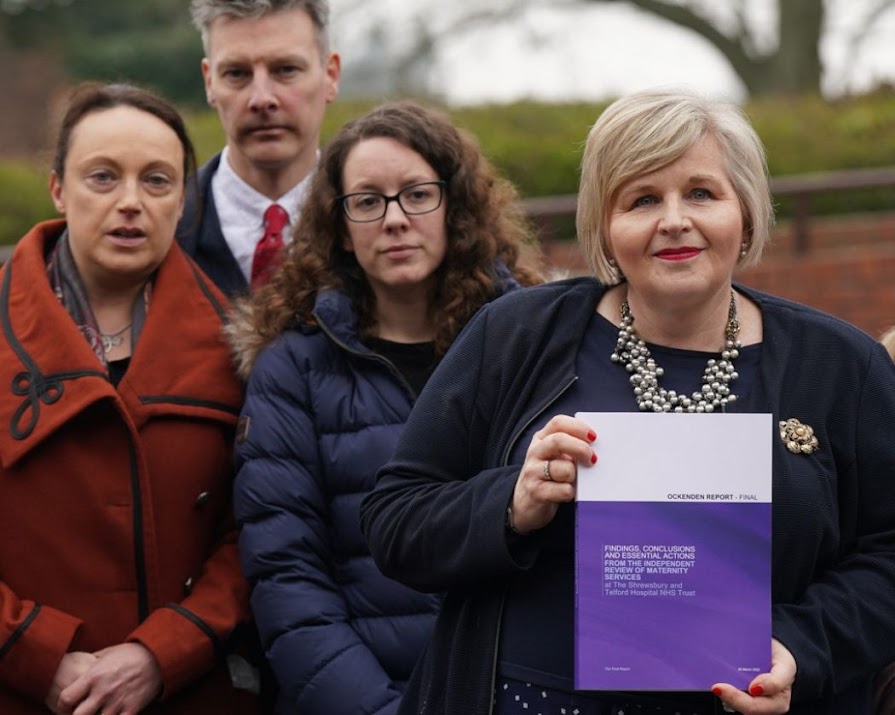
Damning Ockenden report finds that 201 babies could have survived with better care, bringing the biggest maternity scandal in NHS history to light
By Sarah Gill
02nd Apr 2022
02nd Apr 2022
An independent review of maternity services at the Shrewsbury and Telford Hospital NHS Trust has prompted a police investigation into 600 cases and a government apology.
Conducted by maternity expert Donna Ockenden, the shocking report has uncovered hundreds of cases in which healthcare officials failed to undertake serious incident investigations, while deaths were dismissed entirely. The unprecedented size and scale of the review heard from families and staff as it examined baby deaths, condemning the NHS for repeatedly ignoring their own catastrophic mistakes for decades.
“After reviewing the experiences of so many families, and listening carefully to both those families and to the past and present staff who came forward,” Ockenden writes in the report. “We have been given a once-in-a-generation opportunity to improve the safety and quality of maternity service provision for families across England – now and in the future.”
Commencing in 2017, the independent and multi-professional team of midwives and doctors reviewed the maternity care of 1,486 families, the majority of which were patients at the trust between the years 2000 and 2019. Given that certain families had multiple clinical incidents, a total of 1,592 were up for review, with the earliest case from 1973 and the latest from 2020.
The findings of the Ockenden report
In her Letter to the Secretary of State for Health and Social Care, Ockenden wrote, “This final report… is about an NHS maternity service that failed. It failed to investigate, failed to learn and failed to improve, and therefore often failed to safeguard mothers and their babies at one of the most important times in their lives.”
The review was requested by the former Secretary of State for Health Jeremy Hunt after the tireless efforts and commitment of a group of parents whose children lost their lives while in the care of the trust. The largest inquiry into a single service in the 75-year history of the NHS, its findings were truly appalling.
According to the review, babies were stillborn, died shortly after birth or were left severely brain-damaged. Some babies suffered skull fractures, broken bones or developed cerebral palsy after traumatic forceps deliveries. Other newborns were starved of oxygen and experienced life-changing brain injuries, and of the 498 stillbirths examined, 1 in 4 cases were found to have significant or major concerns in maternity care that, if managed appropriately, might or would have resulted in a different outcome.
“In total, 12 cases of maternal death were considered by the review team. They concluded that none of the mothers had received care in line with best practice at the time and, in three-quarters of cases, the care could have been significantly improved.”
A government apology
Addressing the report in parliament, British Health Secretary Sajid Javid issued an apology for these failings. “We entrust the NHS with our care, often when we’re at our most vulnerable. In return we expect the highest standards. But when those standards are not met, we must act firmly, and the failures of care and compassion that are set out in this report have absolutely no place in the NHS. To all the families that have suffered so gravely, I am sorry.”
“The report clearly shows that you were failed by a service that was there to help you and your loved ones to bring life into this world,” he added, vowing to implement the report’s recommendations and ensure the police investigation — Operation Lincoln — leaves no stone unturned.
Learning and improvement
While the combination of favouring natural births over caesarean sections and a lack of oversight are potential roots of these systemic failures, Ockenden pinpoints nine areas for learning at the trust, including management of patient safety, patient and family involvement in care and investigations, complaints processes, and staffing.
Given that a number of the issues highlighted in the report are not unique to Shrewsbury and Telford Hospitals NHS Trust, the review team also identified 15 areas as immediate and essential actions that should be considered by all trusts in England providing maternity services.
These include “the need for significant investment in the maternity workforce and multi-professional training, suspension of the midwifery continuity of carer model until – and unless – safe staffing is shown to be present, [and] strengthened accountability for improvements in care among senior maternity staff, with timely implementation of changes in practice and improved investigations involving families.”
While Louise Barnett, the chief executive at the Shrewsbury and Telford hospital NHS trust, has offered “wholehearted apologies for the pain and distress caused by our failings as a trust,” Kayleigh Griffiths – whose daughter Pippa died in 2016 – said words from the trust “aren’t going to be enough.”